The omicron variant has created a shifting landscape of COVID-19 treatment and prevention possibilities for long-term care clinicians, with major changes occurring over the winter holidays.
Among the breaking clinical news developments in December:
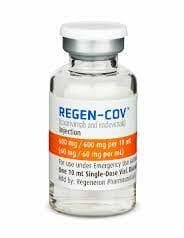
Feds halt allocation of REGEN-COV, other key monoclonal antibody treatments: Federal officials have halted further allocation of certain monoclonal antibody drugs that have been key to long-term care clinicians’ COVID-19 treatment protocol for vulnerable residents. Distribution of the bamlanivimab and etesevimab together, etesevimab alone, and REGEN-COV have been put on pause, the Assistant Secretary for Preparedness and Response (ASPR) and the Food and Drug Administration announced on Dec. 23. New COVID-19 variants are able to resist the drugs, according to their makers. Officials are awaiting updated data from the CDC before deciding on next steps, ASPR said.
In the meantime, federal authorities are scrambling to provide the one monoclonal antibody treatment recently shown to work against omicron. There are 55,000 doses of sotrovimab (brand name Xevudy) currently being allocated, and an additional 300,000 doses of the drug will be available for distribution in January, ASPR said.
Two COVID-19 pills authorized for emergency use: In a pandemic first, the FDA has authorized two oral drugs to be prescribed to adults and children who have mild-to-moderate COVID-19 and are at high risk for progression to severe illness, including hospitalization or death.
Pfizer’s Paxlovid (nirmatrelvir tablets and ritonavir tablets, co-packaged), was authorized on Dec. 22. It is the preferred clinical choice by federal health officials, having been shown to reduce hospitalization risk by up to 90% in clinical trials. Merck’s molnupiravir, authorized for use on Dec. 23, is about 30% effective against hospitalization risk in comparison. It should only be used in cases where alternative authorized COVID-19 treatment options are “not accessible or clinically appropriate,” according to the FDA.
Each drug should be initiated “as soon as possible after diagnosis of COVID-19 and within five days of symptom onset,” the FDA said. Supply appears to be tight and varies from state to state, according to one recent report.
J&J booster cuts healthcare worker hospitalizations in South Africa, researchers say: Research in South Africa shows that the Johnson & Johnson COVID-19 vaccine booster may be effective against the omicron variant. A study of 69,000 healthcare workers during the rise of omicron in that country showed that workers vaccinated with two doses of the vaccine were 85% less likely to be hospitalized when compared to their peers who had received only one dose, according to a National Public Radio report.
On Dec. 17, the Centers for Disease Control and Prevention endorsed a recommendation that Americans preferably be vaccinated with the Pfizer-BioNTech or Moderna COVID-19 vaccines over Johnson & Johnson’s shot. The CDC’s decision hinged in part on the risk of blood clots seen with the J&J vaccine, and the relatively high level of protection against COVID-19 afforded by the other two options.
Omicron hospitalizations about one-third that of delta; South Africa’s 4th virus wave peaks: More signs that omicron may be less deadly than previous SARS-CoV-2 variants have arisen. Despite the fact that omicron appears to be more transmissible than its delta cousin, it is linked to about one-third less risk of hospitalization, according to researchers in the United Kingdom. Meanwhile, a fourth wave of infections caused by the variant in South Africa, where omicron was first discovered, appears to have peaked, authorities said on Thursday, Dec. 30.
This news is republished from another source. You can check the original article here

Be the first to comment